Veterans are brave individuals who have served their country with honor and courage. But right now many face immense mental health challenges upon returning to civilian life and one of these challenges is suicide.
In 2020, there were 6,146 Veteran suicides. This was an average of 16.8 per day. You can read more right here.
In this article, I am attempting to bring awareness to the alarming rates of veteran suicide, explore underlying factors that may be contributing to this epidemic, and discusses potential strategies and resources available to address and prevent veteran suicide.
The statistics surrounding veteran suicide are deeply disturbing and emphasize the need for an effective solution. According to recent studies done by the U.S. Dept of Veterans Affairs, the suicide rate among veterans returning to civilian life is significantly higher than that of the general population.
Let’s take a look at some contributing factors that may make veterans vulnerable to suicide. PTSD or Post-Traumatic Stress Disorder, depression, anxiety, and other mental health issues often stem from the traumatic experiences and challenges faced during war. The transition from a highly structured and cohesive military environment to civilian life can be overwhelming. This can lead to a sense of isolation and loss of purpose. The stigma surrounding mental health problems coupled with the fear of seeking help can definitely further exacerbate this issue.
As treatments for mental health conditions progress further and further each day, there are more and more options for suicide prevention as well as support for veterans and their families. For information on Veteran crisis support click here.
Government agencies and nonprofit organizations alike need to consider devoting more funds and resources to developing accessible and comprehensive mental health programs that are specifically tailored to the unique needs of our veterans. Providing quality mental health care, including counseling, therapy, and medication, is vital for the treatment of mental health conditions.
Public awareness campaigns should aim to educate society about the challenges faced by veterans and debunk misconceptions surrounding mental health. Normalizing the conversation about mental well-being will hopefully encourage veterans to seek help without fear of ridicule or judgment.
It is important to establish peer support groups. These can be instrumental in providing a sense of camaraderie, understanding, and shared experiences. These initiatives create safe spaces for veterans to connect, share their struggles, and provide mutual support.
In some cases, veterans have reached out for help, but sometimes western medicine doesn’t always have the answers. That’s why some have turned to more alternative medicines such as psychedelic-assisted therapy which you can read about here.
In 2019 retired Navy Seal, Marcus Capone along with his wife Amber started an organization called Veterans Exploring Treatment Solutions or VETS, which is one of the leading organizations focusing on ending veteran suicide and addressing TBI (traumatic brain injury) with psychedelic-assisted therapy.
Another factor that can contribute to veteran suicide is TBI, Traumatic Brain Injury is a significant health concern affecting military veterans. TBI can result from combat-related incidents like blasts, explosions, or other head injuries. While the physical consequences of TBI are well-documented, its impact on mental health, particularly veteran suicide, remains a crucial area of concern.
TBI is known to have profound effects on cognitive, emotional, and behavioral functions. Common symptoms include memory loss, difficulty concentrating, mood swings, anxiety, depression, and post-traumatic stress disorder (PTSD). These mental health challenges are major risk factors for suicidal ideation and behavior among veterans.
If TBI can cause PTSD then the link between TBI, PTSD, and suicide should be obvious but it is important to note that not everyone who experiences a TBI will develop PTSD, and not everyone with PTSD will experience suicidal thoughts or behaviors. The relationship between TBI, PTSD, and suicide is complicated and influenced by a multitude of variables, including pre-existing mental health conditions, social support systems, coping mechanisms, as well as access to comprehensive care.
It is vital that government agencies, nonprofit organizations, and healthcare providers collaborate to ensure a seamless system of care for veterans in need of medical intervention. Coordinated efforts can streamline access to mental health services, facilitate information sharing, and reduce bureaucratic redundancy.
Veteran suicide is an unnecessary tragedy that demands our immediate attention. By understanding the scope of the problem, addressing the contributing factors, implementing preventive strategies, and empowering veterans we can make significant strides in reducing the incidence of veteran suicides.
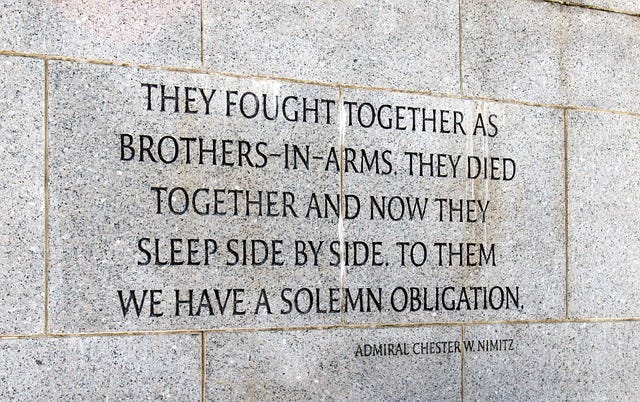
Our collective responsibility as citizens of The United States of America, One Nation Under God, is to provide unwavering support and care for those who have selflessly served their nation, guaranteeing that veterans receive the assistance they need to lead healthy and prosperous lives. Together, we can combat this silent epidemic and honor the sacrifices our veterans have made.







Incredibly important. It's hard to imagine us not taking care of the people who we asked to take care of us.